Towards a digital front door to care



Redefining healthcare access
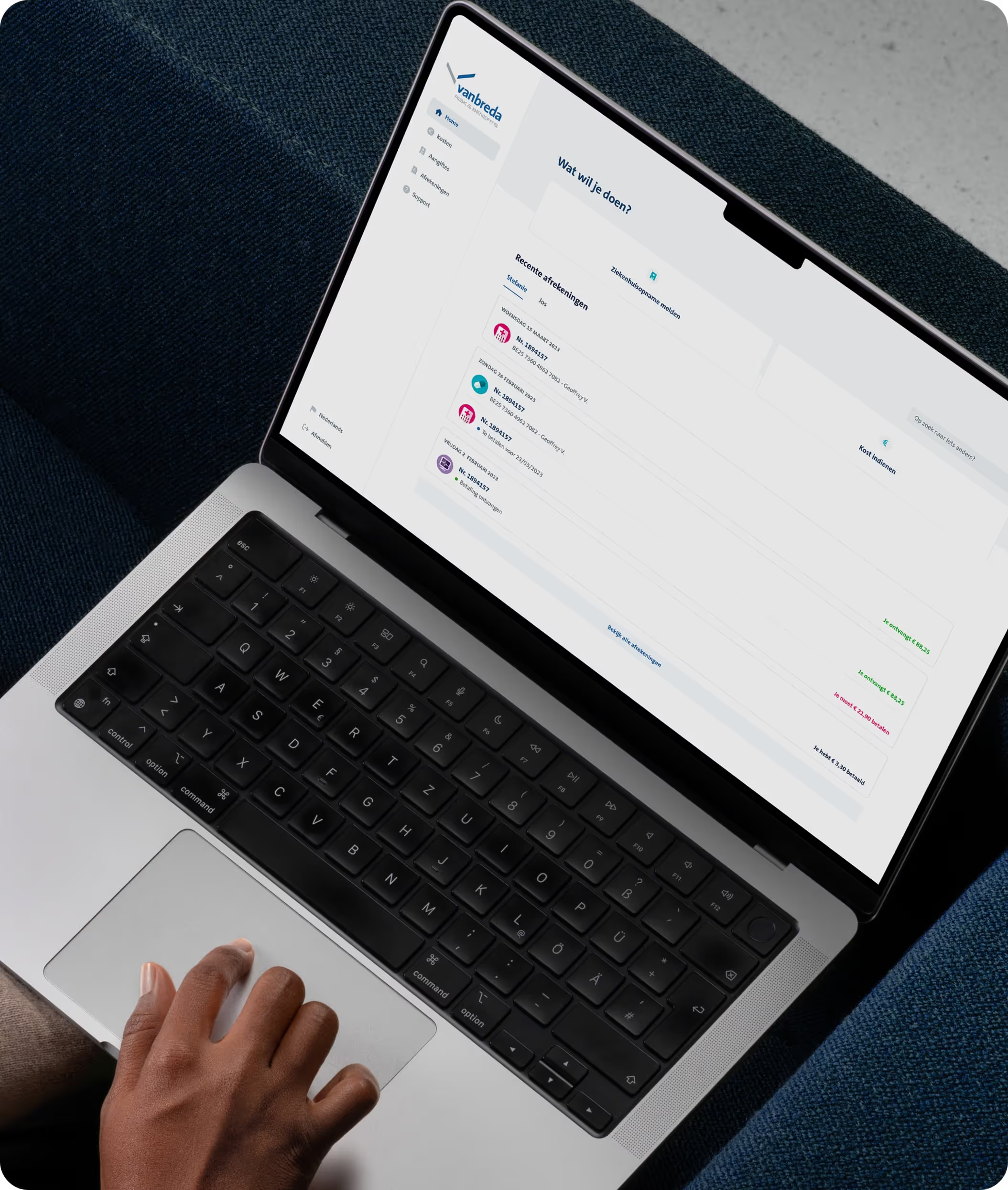
This multi-year partnership involved iterative innovation to provide consumers with streamlined access to healthcare and well-being services while enabling Vanbreda to future-proof their platform for scalability and efficiency.





Bridging the gap between customer needs and business outcomes
For consumers
For Vanbreda Risk & Benefits
Iterative innovation across 4 key phases

Integrating wellness services
To address the growing demand for well-being support, we introduced a dedicated “Wellness Tab” into the web app. This tab provided members with direct access to partner services, such as Doktr for telehealth consultations and BloomUp for mental health support. By seamlessly embedding these services, members were empowered to prioritize their well-being through accessible, insurance-covered options. This integration tested the willingness to use and marked a significant step in making well-being a central part of the digital ecosystem.

Building an omnichannel experience
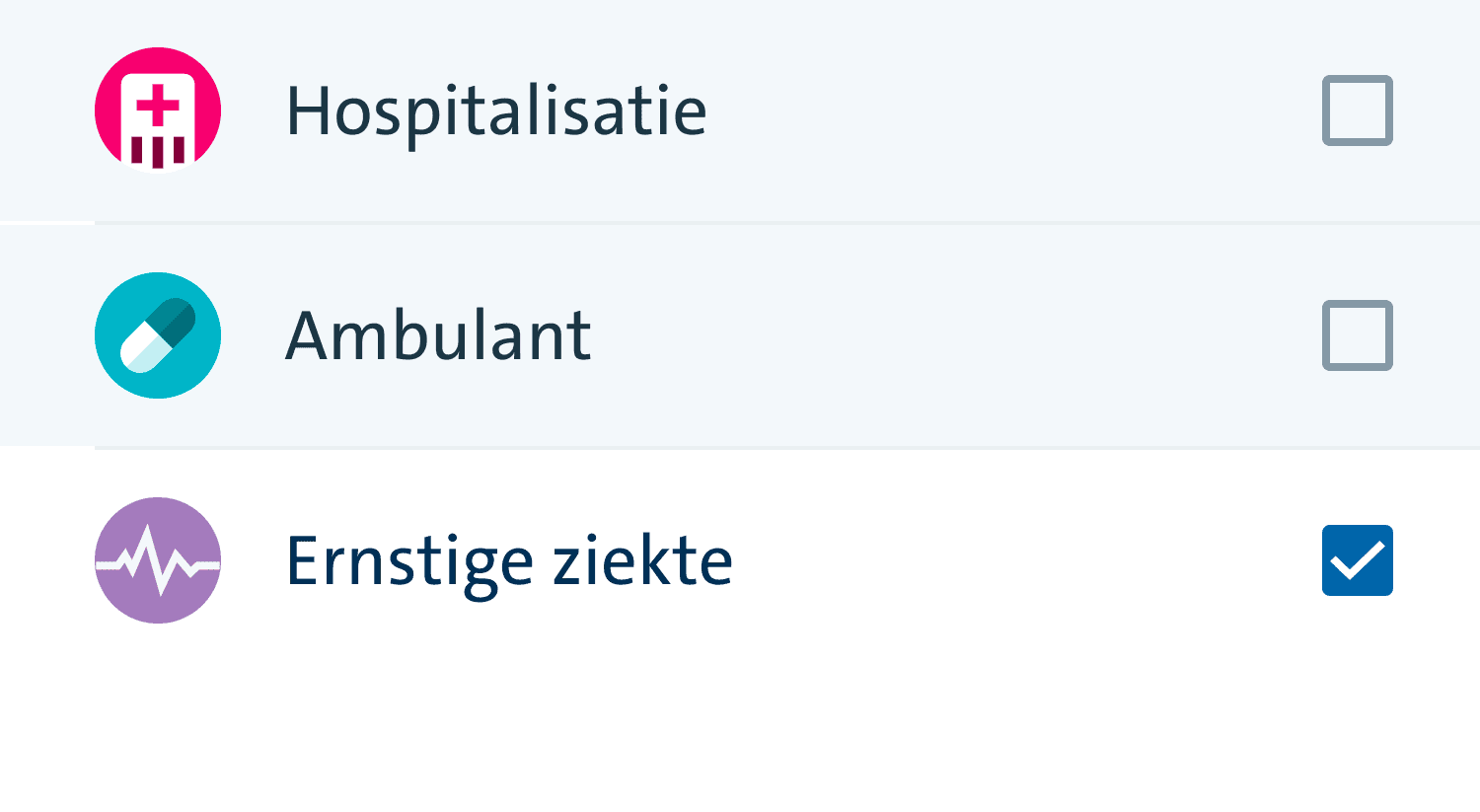
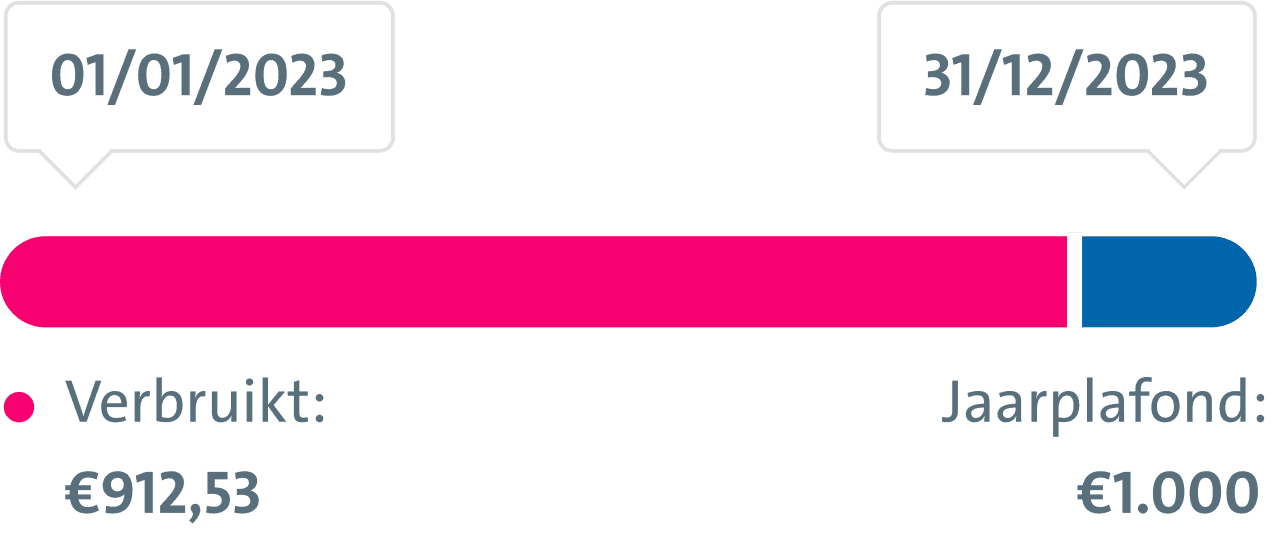
Recognizing the need for accessibility across devices, we developed a web-based platform integrated within a native shell for Android and iOS. This ensured a consistent experience between mobile and desktop. Members could now effortlessly access detailed explanations of policy coverage, reimbursement flows for hospitalization and ambulatory care, and submit claims through an intuitive interface. By adopting this omnichannel approach, Vanbreda eliminated the limitations of a mobile-only solution and expanded their reach to a broader audience.
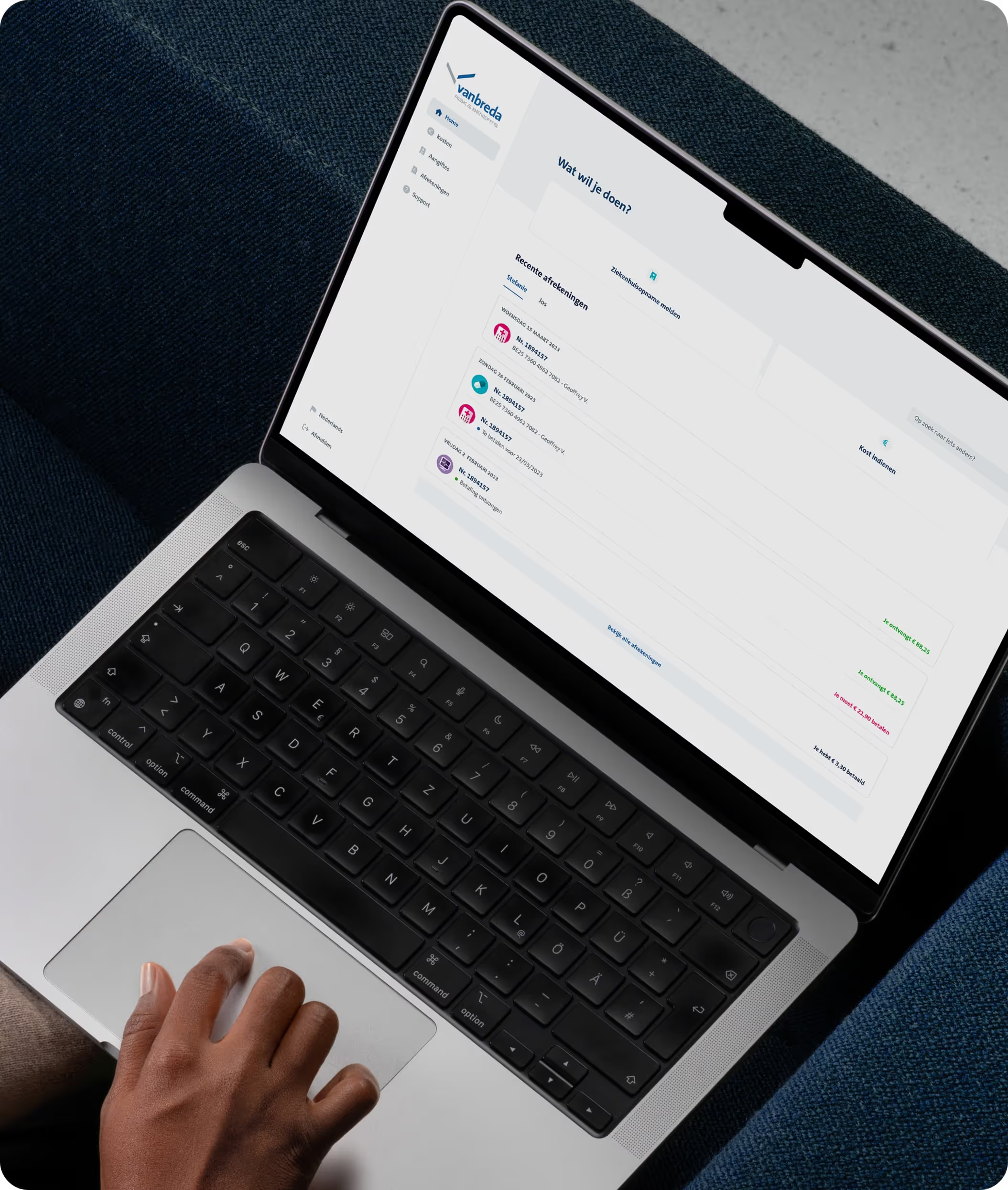
Create modular contact flows
To simplify and accelerate issue resolution, we designed a modular, form-based system tailored to address specific member needs. Whether it involved processing disability claims, resolving hospitalization errors, or handling general inquiries, members could use purpose-built forms for their concerns. This reduced the dependency on manual support channels while significantly improving resolution times. The modular setup allowed for seamless updates and adaptations based on evolving member needs.

White-label branding for TPA clients
As a TPA, Vanbreda needed to provide customizable experiences for their insurer clients. We introduced a white-label platform, enabling insurers to personalize branding and user experiences. Leveraging feature flags, functionalities could be toggled on or off based on each insurer’s requirements, ensuring tailored solutions while maintaining operational simplicity. This innovation positioned Vanbreda as a scalable and adaptable partner for their clients.





Delivering real value
The right things, built right.






A clear path forward for digital healthcare